JACKSON, Miss. (AP) — Top Mississippi lawmakers started negotiating Tuesday on what could become a landmark plan to expand Medicaid coverage to tens of thousands of people in one of the poorest …
Transportation
April marks Distracted Driving Awareness Month, and one company is taking strides to combat the threats of distracted driving through new technology.
Waymo , an autonomous vehicle pioneer owned …
UNITED NATIONS (AP) — The United Nations called Tuesday for “a clear, transparent and credible investigation” of mass graves uncovered at two major hospitals in war-torn Gaza that were raided …
Valley & State
economic development
The city of Peoria wants to use 8,300 acres of Arizona state land across the northern part of the city — a size greater than the Vistancia master-planned community — for a new airpark and other possible future developments.
Election 2024
Maricopa County will have a new permanent sheriff after the November election, no matter who wins.
Former Sheriff Paul Penzone, a Democrat, stepped down in January and Russ Skinner was appointed …
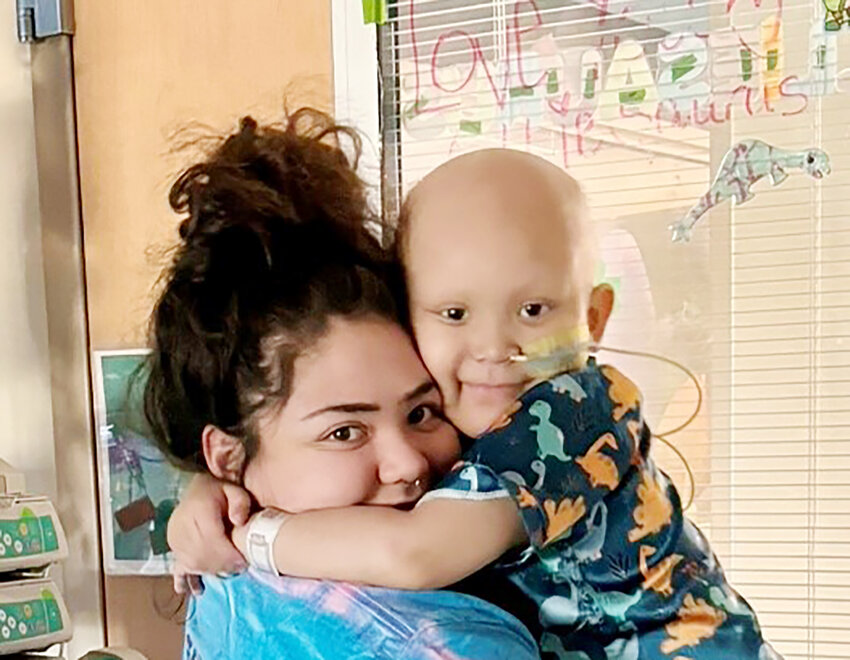
neighbors
While the Arizona Department of Public Safety has not yet provided the result of its investgation into the Jan. 7 fatal pedestrian car accident in the Town of Paradise Valley, the family of late …
ENVIRONMENT
The combination of Arizona Volunteer Week and Earth Day on Monday brought out volunteers April 22 for an adopt-a-highway cleanup effort.
The Arizona Department Adopt a Highway volunteers were …
SENIORS
Attorney General Kris Mayes announced Tuesday that a receiver has been appointed for Heritage Village, an assisted living facility in Mesa.
Maricopa County Superior Court appointed Peter S. …
ON TOUR
Megadeth is bringing its live show to North America with a nationwide fall tour, Destroy All Enemies, which will include a Phoenix stop.
GRAND JURY
Two teens have been indicted in what the Maricopa County Attorney’s Office called an “ambush” shooting of a Phoenix police officer.
Mathew Rodriguez, 17, has been charged as an …
SERVICES
The Arizona Corporation Commission has voted to approve the Luke 303 Wastewater rate consolidation sought by EPCOR, a utility company that manages water, wastewater, natural gas and electricity …
An Arizona judge has declared a mistrial in the case of rancher accused of fatally shooting a Mexican man on his property near the U.S.-Mexico border. Jurors could not reach consensus on last …
Read more



!role~Preview!mt~photo!fmt~JPEG%20Baseline)

!role~Preview!mt~photo!fmt~JPEG%20Baseline)








!role~Preview!mt~photo!fmt~JPEG%20Baseline)






!role~Preview!mt~photo!fmt~JPEG%20Baseline)
!role~Preview!mt~photo!fmt~JPEG%20Baseline)
!role~Preview!mt~photo!fmt~JPEG%20Baseline)
!role~Preview!mt~photo!fmt~JPEG%20Baseline)
!role~Preview!mt~photo!fmt~JPEG%20Baseline)















!role~Preview!mt~photo!fmt~JPEG%20Baseline)
!role~Preview!mt~photo!fmt~JPEG%20Baseline)
!role~Preview!mt~photo!fmt~JPEG%20Baseline)
!role~Preview!mt~photo!fmt~JPEG%20Baseline)
!role~Thumbnail!mt~video!fmt~JPEG%20Baseline)
!role~Preview!mt~photo!fmt~JPEG%20Baseline)
!role~Preview!mt~photo!fmt~JPEG%20Baseline)
!role~Preview!mt~photo!fmt~JPEG%20Baseline)
!role~Preview!mt~photo!fmt~JPEG%20Baseline)
!role~Preview!mt~photo!fmt~JPEG%20Baseline)
!role~Preview!mt~photo!fmt~JPEG%20Baseline)
!role~Preview!mt~photo!fmt~JPEG%20Baseline)
!role~Preview!mt~photo!fmt~JPEG%20Baseline)
!role~Preview!mt~photo!fmt~JPEG%20Baseline)
!role~Preview!mt~photo!fmt~JPEG%20Baseline)
!role~Preview!mt~photo!fmt~JPEG%20Baseline)
!role~Preview!mt~photo!fmt~JPEG%20Baseline)